“There are three areas to improve evidence-based clinical care to reduce the rate of CAUTI [Catheter-Associated Urinary Tract Infections]: (1) prevention of inappropriate short-term catheter use, (2) nurse-driven timely removal of urinary catheters, and (3) urinary catheter care during placement. Nursing screening and assessment and evidence-based management of urinary retention and incontinence is essential to reduce catheter overuse. ANA [American Nurses Association] identified the opportunity to fill the tool gap and develop a steam lined evidence-based tool to reduce CAUTI …
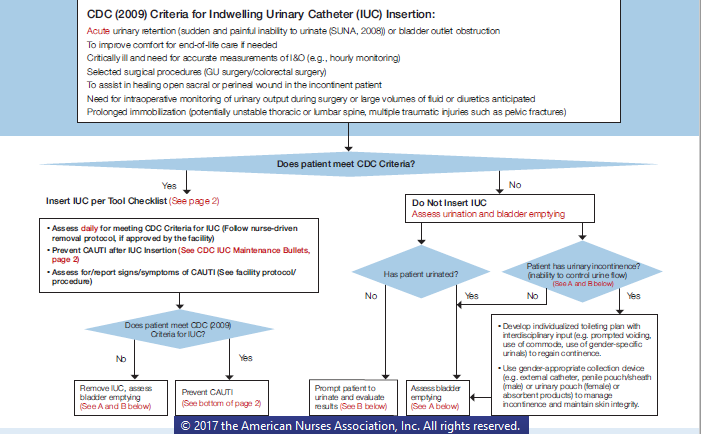
Nurse consultants from the PfP [Centers for Medicare and Medicaid Services (CMS) Partnership for Patients] team and representatives from CDC [Centers for Disease Control & Prevention] were included in the panel. After extensive review of evidence-based guidelines, existing CAUTI reduction tools, and a focused review of the literature, ANA and other TEP [Technical Expert Panel] members developed a two-part multi-factorial CAUTI reduction tool designed for nurses … The one-page tool is based on the CDC’s 2009 ‘Guideline for Prevention of Catheter-Associated Urinary Tract Infections.’ … The evidence-based tool incorporates an algorithm to determine if a urinary catheter is appropriate based on nursing screening and assessments, as well as alternatives for retention and incontinence; timely removal; and a checklist on catheter insertion, cues for essential maintenance and post-removal care.
It is important that hospitals implement multiple successful ‘levers’ that have been identified by the PfP and in the literature to successfully reduce CAUTI in addition to consistent use of the ANA CAUTI Prevention Tool. The ANA tool is essential to use as an effective practice change lever and is an important innovation to drive evidence-base care. In addition, additional levers have been identified including a safety culture, nurse-driven catheter removal (standing orders per protocols), incorporation of health information technology (e.g., clinical decision support and nurse protocols seamlessly cued to nurses in electronic health records), consultation by specialty nurses (e.g., nurses certified in wound, ostomy and continence nurses, urology, rehabilitation, infection control, geriatrics), and effective team-based programs such as Comprehensive Unit-based Safety Program (CUSP). By using multiple levers simultaneously, a tipping point to achieve reduction in the nation’s CAUTI rate can be achieved to save lives, prevent harm and reduce cost.”