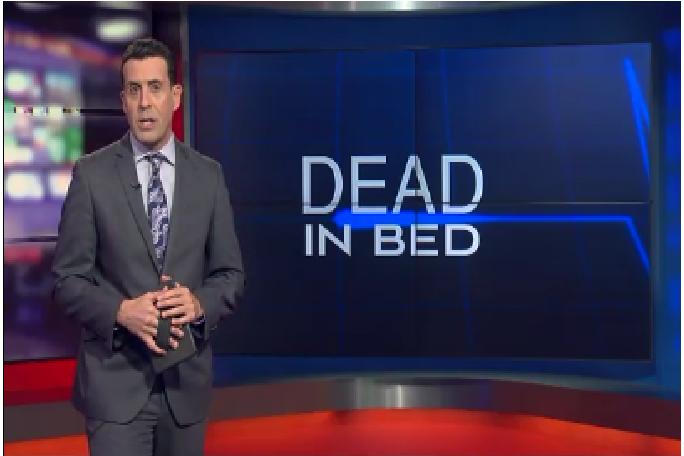
“‘Dead in Bed’ is the culmination of a five-month investigation by the On Your Side News 5 investigative team that began with questions raised by an Ohio husband. Marty Schmidt said goodnight to his wife in a hospital room only to learn she died hours later. How could patients undergoing “successful’ surgery and assigned to “low risk” floors, suddenly die within hours? We interviewed some of the nation’s most respected medical experts from Washington D.C. to Indianapolis and Dallas. Plus, we spoke with families in Ohio, Indiana, Georgia and California whose loved ones died. What we uncovered is one of medicine’s best kept secrets.”
The avoidable death syndrome summarized in the foregoing quotation and described in the source video (http://www.newsnet5.com/longform/dead-in-bed-a-deadly-hospital-secret?utm_source=Join+the+Patient+Safety+Movement&utm_campaign=375b6c4b6a-EMAIL_CAMPAIGN_2016_12_23&utm_medium=email&utm_term=0_f03e80c12e-375b6c4b6a-) is exacerbated by the increase in prescribed opioid use, which contributes to positive patient satisfaction and hospital revenues but which increases the potential for overdose and consequent respiratory failure. Constant cardiovascular monitoring, which technology is cost-effective but typically employed only in post-operative and intensive care hospital units rather than convalescent units where most “dead in bed” patient adverse events occur, can be easily and cost-effectively employed hospital-wide using the application/”app”-building capability provided by cloud-based information technology (IT) that conforms to the Cloud Healthcare Appliance Real-Time Solution as a Service (CHARTSaaS) reference architecture, as described in the two presentations at these URLs:
CHARTSaaS, accessible by subscription in the cloud to minimize cost and complexity, provides the tools and methods for healthcare provider subject matter experts (SMEs) with little or no IT staff assistance to leverage already installed a.k.a. “legacy” electronic health record (EHR) systems and other ancillary systems and services to implement constant monitoring of all patients via pulse oximeter or other bedside monitor device data streams. Parameters for monitoring and patient-/case-specific threshold values and/or time-related criteria can be included in rules for use by continuously operating (24 X 7 X 365) processes, which can notify specific staff by name or role via whatever digital device is most convenient instantly when the parameter value conditions are met. Therefore, this specific example of the general patient adverse event type called “failure to rescue” can be mitigated, saving an estimated 5,000 patient lives per year!