N.B. — This post is one in a series of ten, based on Becker’s Infection Control & Clinical Quality article 10 top patient safety issues for 2017 by Heather Punke & Brian Zimmerman and published on January 18, 2017 (http://patientsafetymovement.org/challenges-solutions/actionable-patient-safety-solutions-apss/).
“Catheter-associated urinary tract infections [CAUTI]. A report on the CDC’s Winnable Battles initiative released Dec. 5 showed strong progress in the reduction of hospital-associated infections, with one exception: catheter-associated urinary tract infections. Although previous studies suggest as many as 69 percent of CAUTIs are preventable, the infection continues to prove problematic for hospitals.
CDC began Winnable Battles in 2010 and set ambitious goals to be reached by 2015. The results show targets of 60 percent reductions in both central line-associated bloodstream infections and invasive methicillin-resistant Staphylococcus aureus infections are on track to be achieved. Additionally, achieving the target of a 30 percent reduction in surgical site infections looks to be feasible. However, the target of reducing CAUTIs in acute care hospitals by 30 percent was not reached. While CDC data did show a 24 percent decrease of CAUTIs in hospital wards, hospital intensive care units saw a 16 percent increase in CAUTI occurrence.
However, a recently published study examining the efficacy of a CAUTI reduction collaborative effort supported by the Agency for Healthcare Research [& Quality, AHRQ] shows promise. The initiative provided Quality Comprehensive Unit-based Safety Program toolkits for CAUTI reduction to physicians and nurses across 603 hospitals. Program adherence was associated with a reduction of approximately one-third for CAUTIs in general wards …”
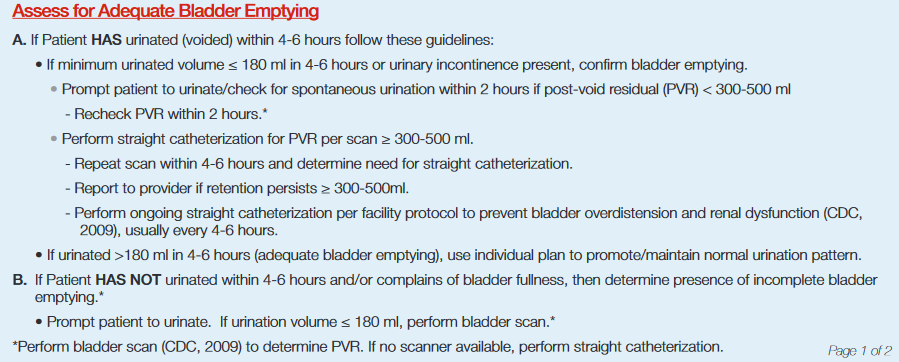
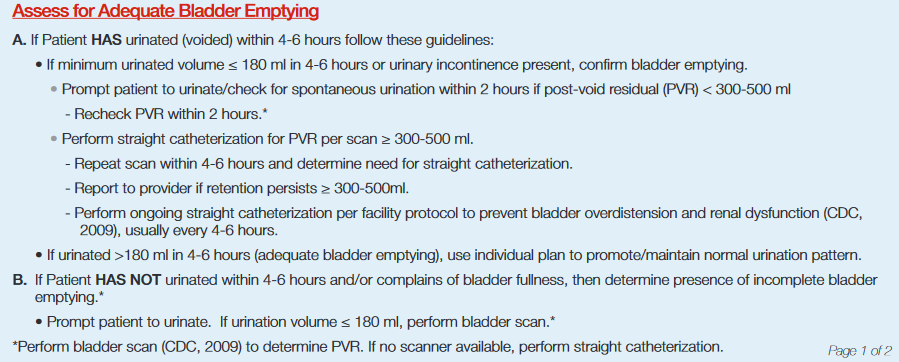
The foregoing quote from the Becker’s Infection Control & Clinical Quality e-publication includes a reference to the AHRQ-supported immunization strategies. One such strategy is the American Nursing Association (ANA) CAUTI Prevention Tool (informed by Guidelines for Prevention of CAUTI of the U.S. Centers for Disease Control & Prevention a.k.a. CDC, 2009) is based on an intricate and data-dense flow chart that prescribes nursing actions to implement these key practice strategies: “1) Fewer Catheters Used, 2) Timely Removal and 3) Insertion, Maintenance and Post-Removal Care” (http://nursingworld.org/ANA-CAUTI-Prevention-Tool). Although the purpose of the flow chart document is to simplify clinical staff adherence to a simple but time-critical and data-driven process, it is evident from the three process content category names — “Algorithm Section, Indwelling Urinary Catheter (IUC) Insertion Checklist, Maintenance of IUC/Drainage System and Other Patient Care to Prevent CAUTI” — that this process is likely to exceed human cognitive capabilities to conform in the context of the plethora of processes that operate concurrently in a typical healthcare delivery venue such as a hospital floor/ward.
By applying an appropriate information technology (IT) that is compliant with the Cloud Healthcare Appliance Real-Time Solution as a Service Reference Architecture (CHARTSaaS RA), the complex and time-critical CAUTI protocol can be automated in a manner that drives timely execution of the ANA-prescribed CAUTI-prevention process by prompting staff to execute the required actions at the required times based on automatic monitoring of critical and patient-specific parameters as specified in the protocol, as in this example:
Please validate the automated protocol/process proposition to your own satisfaction by reviewing the details of CHARTSaaS and the CHARTSaaS RA in these presentations, and then by imagining a CHARTSaaS-enabled IT solution:
Healthcare providers and their patients will benefit significantly from appreciating and then applying a CHARTSaaS RA-compliant IT solution. To do so will mitigate medical mistakes (currently the third leading cause of patient deaths, per Makaray and Daniel, http://www.bmj.com/content/353/bmj.i2139), thereby minimizing patient adverse events; and also will optimize clinical case outcomes while maximizing the cost-effectiveness of care and treatment and accelerating the accrual of medical knowledge.