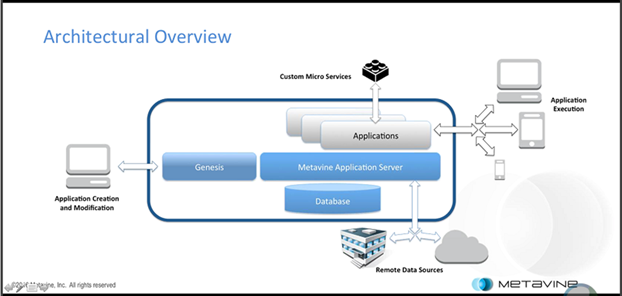
N. B. — The title graphic depicts all the essential components of the CHARTSaaS RA, provided that they are implemented in a HIPAA-compliant Internet “cloud” environment and accessible only to accredited and licensed healthcare provider subscribers via a secure portal.
An article authored by Martin Makary, MD, of Johns Hopkins Medicine, published in May of 2016 in The British Medical Journal, reported on a study recently completed by Dr. Makary and a co-author, which determined that medical errors now constitute the third most frequent cause of patient deaths in the United States. Exceeded only by heart disease and cancer, medical errors lead to the deaths of approximately one-quarter million patients in 2013. Although much of the attention attracted by this article was focused on the validity of the results reported, a more problematic and critical focus should be on the nature of these medical mistakes and how to mitigate them.
Cognitive complexity of medical practice and healthcare delivery
The practice of medicine and delivery of healthcare incorporate the target pathology, the patient who manifests the pathology, and the physician or other healthcare provider who seeks to determine the nature of the pathology and the best (that is the most effective, efficient and economical) means of pathology treatment and patient care. The symptoms with which the patient presents, as solicited by the provider and reported by the patient as the patient history, are the subjective impressions of the target pathology (which may include one or more distinct illnesses). The signs that the provider detects through the physical examination and possibly confirming test results are the objective manifestations of the presenting patholog(ies). The provider’s purpose is to determine and delivery care and treatment to reduce or eliminate the pathology and thereby return the patient to a more typical or normal physiological equilibrium a.k.a. homeostasis.
The human body works continually to maintain a steady biochemical state of life-critical parameters as required to enable normal interoperability of molecules and cells and tissues and organs and systems for the survival of the human individual. When the individual’s bio-physiological state is forced out of equilibrium by an abnormal circumstance such as introduction of an infectious agent or physiological event such as autoimmune system malfunction, then a disease state is created. If the body cannot reestablish healthy equilibrium through operation of its homeostatic control “micro” mechanisms, then the health of the individual as a whole degrades. When the clinical symptoms are observed, medical intervention is required. Ideally, constant monitoring should operate to detect the human individual’s approach to a high risk state, and to invoke medical intervention to avoid active disease, as shown in the “macro” section of the slide. Significant healthcare costs arise from the failure to detect and react to pathological events soon after they occur, thus allowing progression to the active disease state in which only 20% of the population generates 80% of health system costs.
Not only is timeliness of the essence, at both the micro and macro extremes described above; but also it is critical for success in each of the four healthcare subdomains:
1.personal health management, including the full duration of human life from conception to death and post-mortem characteristics (a.k.a. womb-to-tomb);
2.medical practice (a.k.a. outpatient episode-of-care) support, typically of several weeks to several months duration, including creation of a patient- and case-specific differential diagnosis from which a final diagnosis is made, and treatment planning for the principal presenting pathology and/or undiagnosed problems;
3.healthcare delivery operations (typically an general hospital length-of-stay of typical several days but occasionally several months duration), including care and treatment activity and also provider organization resources and facilities management, as defined in the USA by accreditation standards of The Joint Commission (TJC); and
4.accruals to the medical common-body-of-knowledge for application to next/new episode of care with greater clarity and correctness.
These four subdomains of medical practice and healthcare delivery are complicated by several inherent domain characteristics including professional complexity, lack of comprehensive standards, minimal use of state-of-the-art information technology or “IT” tools and methods, a multi-agency basis for laws and regulations, the disparate array of practice/delivery venues and accompanying variation in standards, practices and the mix of medical art and science, the complexity of facilities and equipment, often operated by certified others for testing & treatment on the patient’s principal provider’s behalf.
In addition to the domain-based challenges of healthcare provider professional activity, these characteristics of clinical practice complicate and therefore degrade cognitive functioning:
- healthcare delivery venues are complicated because of
- multi-disciplinary teams of various provider professions,
- multiple methods and specialty bodies of knowledge,
- a plethora of concurrently operating processes;
- a patient episode of care or case actually is a scientific experiment but performed under uncontrolled conditions;
- case-related information is extreme in its volume, variety, velocity, variability and is inconsistent in its veracity; and it emanates from various sources at unpredictable times; and
- the “bridge from bench to bedside” is problematic because relevant findings occur randomly and are difficult for providers to acquire, assess, apply and adapt in real-time as patient care requires.
The challenging healthcare provider domain and practice characteristics just described are exacerbated by ambient or domain environmental conditions and also professional provider personal situations. All of the major characteristics listed on this slide lead to cognitive overload, resulting in degradation of even the super-median levels of memory and reasoning with which the typical clinician presents. Among these exacerbating characteristics are high decision density, interruptions or distractions, circadian dys-synchronicity (uncoordinated/conflicting psychological and physiological states within a daily time period), fatigue, emotional perturbations a.k.a. affective state (which alludes to conflict in pre-frontal lobe and limbic system-provoked behaviors), and sleep deprivation (which as described in the foot note can mimic other clearly clinical conditions that professional standards prohibit).
The confluence of healthcare provider personal and operating domain characteristics we have reviewed are the basis for a far greater than acceptable degree of recurring medical mistakes, increasing at an accelerated rate to date; which mistakes have become the basis for many professional and popular press publications, many of which include taxonomies of medical mistake or error types and correlation with so-called patient adverse events or PAEs – a euphemism for iatrogenic or nosocomial increases in patient morbidity (illnesses) and mortality (deaths). It is time to cease studying and bemoaning the circumstances of provider-caused illness and death, and to begin developing medical mistake mitigation methods using currently available and cost-effective computerized capabilities. The focus of this development effort should on cognitive support for healthcare providers in the practice of medicine and delivery of healthcare; because, as previously demonstrated, clinical cognitive overload arguably is the root cause of medical mistakes.
One may visualize human clinical cognitive capability as a rapidly recurring cycle of four specific information-based activities: first, to acquire; second, to assess; third, to apply; and fourth, to adapt. This cycle is in fact a so-called feedback loop; whereby the acquired and assessed information is applied to some activity or circumstance, and then the results are interpreted and applied to the activity to modify usually to improve the results previously obtained. Concurrent conduct of this cognitive capability for many processes for many patients on a continuing basis without error exceeds the cognitive capacity of a clinician or even a clinical care delivery team. However, zero-defect recurring and concurrent operation of these activities and tasks are well within the capability of computers, provided that the hardware and software components are appropriately architected and accessible. In fact, such a configuration of computer capabilities could not only ensure reproducible (i.e. – error free) recurrence but also could accelerate stochastic optimization to create a kind of self-learning artificial intelligence capability to accelerate accrual and application of new knowledge. This in turn would accelerate the progression from the iterative/experimental mode of treatment, for currently poorly understood pathology such as infrequently occurring forms of cancer; to the sequential/prescriptive mode, for well-understood pathology such as Type II Diabetes.
Providing cognitive support to mitigate medical mistakes
To date, the extent of cognitive support for healthcare improvement has been limited to the most part to process efficiency improvement methods and tools originally applied in the manufacturing industry, generally known as Lean or Six-Sigma. The essence of these protocols is to recognize and remove extraneous, complicating and/or costly steps from targeted processes, document the refined processes and train domain experts in their content and application. In fact, the applicability and potential benefit of these protocols have been recognized by several industries including healthcare providers; on behalf of which Mark Chasin, MD, President & CEO of The Joint Commission, developed and published a paper describing a variation on the Lean/Six-Sigma approach named Robust Process Improvement (RPI).™ Medical practitioners and researchers have taken this approach a step further toward simplification and reliable replication with the check list approach, best know of which are Atul Gawande, MD, at his Harvard- and Brigham & Womens Hospital – affiliated Ariadne Labs; and Peter Pronovost, MD, PhD, at his Johns Hopkins Medicine-based Armstrong Institute.
However, all these approaches exhibit two medical practice detriments. First, the move toward simplification runs the risk of glossing over what may be a multiplicity of medical critical considerations, as typified for example by the approximately 250-page CDC protocol for arresting the usually rapid and often fatal progression from sepsis to septic shock; and second, that the need to learn, memorize and recall unpredictably even a short check-list exacerbates the root cause of medical mistakes –- cognitive overload. The alternative to Lean/Six-Sigma protocols is an IT-based aggregate of tools and methods, whereby documentation still is a necessary precursor. However, the derivative deliverable is not a documented process to be memorized and recalled at a moment’s notice but, rather, a process memorialized in easily modifiable software that has been designed in a customized manner by the concerned provider and is operable continuously or on demand or automatically upon occurrence of pre-defined conditions; and which runs in a manner that ensures error-free replication. Thus, every patient case receives equally expert diagnosis, treatment and ongoing care.
The computerized capability configuration required for medical mistake mitigation can be described as a cloud-based intelligent business process management suite. Both the cloud service provider (CSP, re https://www.gartner.com/doc/3159939/market-guide-cloud-service-providers) and the intelligent business process management suites (iBPMS, re https://www.gartner.com/doc/reprints?id=1-3F1C5YC&ct=160817&st=sb) are state-of-the-art IT approaches but nevertheless are well-understood, commercially available and widely used globally in several industries other than healthcare. A detailed description of commercial off-the-shelf (COTS) components with or without custom coding to satisfy a particular requirement set or purpose is called in IT jargon a “reference architecture (RA).” The components, configuration and capabilities of a cloud-based intelligent business process management suite for cognitive application a.k.a. “app” creation is named the Cloud Healthcare Appliance Real-Time Solution as a Service (CHARTSaaS), described according to its acronym thus:
- Cloud-based – a solution-as-a-service (SaaS) capabilities accessible anytime and anywhere via a secure portal,
- Healthcare – to support the extreme non-functional/system and functional/capability requirements of healthcare domain,
- Appliance – to provide capabilities for application/”app” creation with minimal subscription cost and IT complexity, and
- Real-Time – to enable analytics-based cognitive support use case time-sensitive and randomly occurring operation (e.g. – physiological device monitoring, immediate post-workup differential diagnosis)
Here is a more complete presentation of CHARTSaaS:
A CHARTSaaS RA-compatible IT solution
The cloud platform portion of the CHARTSaaS RA principally satisfies the system-level or non-functional requirements (i.e. — requirements common to all features and function supported by the solution) such as security, availability and scalability. Specifically, security is provided in satisfaction of the United States of America Federal Health Insurance Portability and Accountability Act (HIPAA) Privacy and Security Rule requirements pertaining to the logic and data platform; networking and access authorization. Also included on a suitable CSP platform are these features:
- configurable connectors for connectivity via the Internet to various commercially available and widely installed subscriber electronic health record or EHR systems a.k.a. hospital information systems, such as Epic, Cerner and MEDITECH;
- software development kits or SDKs and also the CHART integrated development environment or IDE, for application development and/or connectivity to subscriber/end-user applications; and
- SDKs for connectivity or configurability of Internet of Things or IoT mobile and wearable devices.
Here is a more complete presentation of the CHARTSaaS RA:
Satisfaction of the application or functional requirements are provided by the iBPMS portion of the CHARTSaaS RA. The fundamental component is the secure (per Health Insurance Portability and Accountability Act or HIPAA Privacy and Security Rule requirements) healthcare integration or enterprise service bus (ESB). This communication channel provides access among the components of the Suite and data sources, systems and applications with which apps built using the CHARTSaaS RA-compatible solution must connect and communicate. The suite components include the design, development and run-time or operations processors for complex events monitoring and analysis, Boolean and table-driven decisions, Bayesian and multi-variate natural language data set searching, similarity and predictive analytics, and administrative and clinical processes composed of activities/tasks to be performed by system and staff actors. A CHARTSaaS RA-compatible IT solution as an integrated development environment is a tool to develop and deploy applications/apps that provide cognitive support by running in conjunction with installed or legacy applications and leveraging their functionality.
The procedure for using a CHARTSaaS RA-compatible IT solution to design, develop and deploy a medical or healthcare provider process app includes these six steps:
1.Subscribe to the solution, create an account and login.
2.Describe the target process using the blueprint/flowchart with low-/no-code tools and techniques such as drag-and-drop.
3.Generate application code automatically from blueprint or flowchart with little or no IT staff assistance.
4.Define connectivity to subscriber and/or Web-accessible systems and sources of data required by subject process.
5.Deploy and launch process for immediate and continuous operation or on-request or conditional use.
6.Assess process operation manually or automatically, using activity monitoring feature, and modify as/if needed for continuous process improvement over time.