Prompted by a recent New England Journal of Medicine (NEJM) Perspective article describing healthcare transformation,[1] and motivated by a recent study identifying medical mistakes as the third leading cause of death in the United States of America,[2] CHARTSaaS.org, a United States not-for-profit corporation (www.chartsaas.org), posits that now is the time to recognize and to act on the unique potential of state-of-the-art information technology (IT), innovatively employed, to effect the optimization of medical practice and healthcare delivery in a manner that will mitigate medical mistakes and save patient lives. This IT-enabled optimization of healthcare provider practices can be accomplished by minimizing the arguably root cause of patient adverse events – cognitive overload. Consistent with the call previously published in NEJM[3] to adopt an “… IT foundation required for health care … [including] the core set of health data types, the formalization of health care workflows, and encoded knowledge (e.g., practice guidelines, decision-support tools, and care plans);” we propose a low-cost and minimally complex approach for implementing the required “IT foundation for health care” to realize the customized clinical cognitive support on which the long-overdue positive transformation of healthcare depends. The recommended IT cognitive support is specified by the Cloud Healthcare Appliance Real-Time Solution as a Service Reference Architecture (CHARTSaaS RA), which describes the IT hardware and software components, configuration and capabilities required for providers to create customized applications, a.k.a. apps, with minimal cost and complexity.
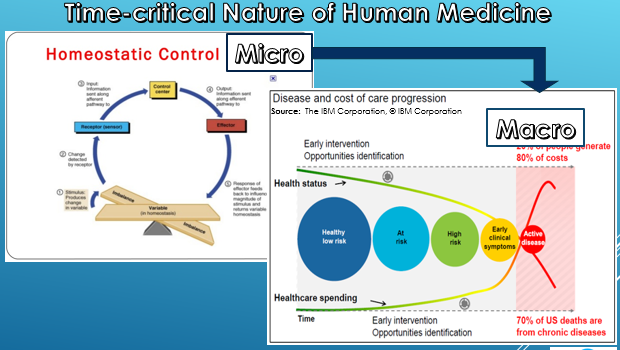
To appreciate the positive potential of the CHARTSaaS RA, clinicians and administrators should reflect on the complexity of the healthcare provider domain in all of its aspects. The object of the domain’s activities is the incompletely understood human body and its inherent and continually changing homeostasis-driven biochemical mechanisms. The complexity of the human body compounds the complexity of effecting the purpose of medicine; which is the diagnosis and treatment of human pathology, the execution of which constitutes a scientific experiment but in uncontrolled conditions. The cognitive challenges thus posed are exacerbated both by the ambient conditions of the typical healthcare provider venue – a plethora of concurrently operating administrative and clinical processes – and by the continually increasing volume, variety and velocity of information. These cognitive challenges are exacerbated by interruptions and distractions, circadian dys-synchronicity, fatigue, emotional perturbations, and sleep deprivation. Compounding all of these conditions are the more insidious considerations of bias, and of cognitive and affective dispositions to respond (CDR/ADR); all of which are described and analyzed elegantly in several popular and professional publications.[4]
Human cognitive capability can be visualized as a rapidly recurring cycle of four specific information-centric activities: first, information acquisition, including constant monitoring and complex event analysis; second, information assessment, including evidence-based case record and other unstructured content similarity searching and predictive analytics; third, information application, including decision-making in the context of purpose-specific process execution; and fourth, information adaptation, including results analysis and knowledge development as the basis for process modification and re-execution. This cycle is a feedback loop; whereby the acquired and assessed information is applied to some activity or circumstance, and then the results are interpreted and applied to the activity as/if indicated for continuous process improvement. However, concurrent operation of the cognitive capability cycle for many processes for many patients on a continuing basis without error exceeds the cognitive capacity of a clinician and even a clinical care delivery team; which creates the risk of medical mistakes and consequent patient adverse events (PAEs).
Nevertheless, zero-defect recurring and concurrent operation of these activities and tasks in the context of continuously operating processes are well within the capability of IT systems, provided that the hardware and software components are appropriately architected and accessible. In fact, such a configuration of computer capabilities could not only ensure reproducible recurrence of error-free processes but also accelerate stochastic optimization to create a kind of self-learning capability, a.k.a. artificial intelligence, to accelerate the accrual and application of new knowledge. These dynamics in turn would facilitate and accelerate the progression from the iterative/experimental mode of treatment for poorly understood pathologies such as forms of cancer to sequential/prescriptive mode of treatment for well-understood pathologies such as Type II Diabetes, as described by Dr. Bohmer[5], the author of the Perspective article cited above.
The computerized capability configuration needed for medical mistake mitigation is described by IT analyst firms[6] as a low-/no-code intelligent business process management suite (iBPMS, which may be thought of as a software development kit, a.k.a. SDK), and is marketed as of this writing by an increasing number of independent software vendors (ISVs). An iBPMS is well-suited to hands-on use by healthcare provider subject matter experts with minimal IT professional staff assistance, because the typical mode of user interaction is via non programing/coding methods such as “drag and drop.” In addition, the iBPMS must operate on an IT platform in the “Cloud” (i.e. – a professionally managed data center accessible via the Internet) that complies with the Health Insurance Portability and Accountability Act (HIPAA) Administrative Simplification Privacy and Security Rules/Regulations and other domestic and international governing laws, regulations and standards; which platform is offered as of this writing by only a few cloud service providers (CSPs). Although the healthcare-oriented CSPs and cloud-based iBPMS represent a niche market and a state-of-the-art IT solution, nevertheless they are well-understood and widely used successfully in several industries other than healthcare globally.
We refer to this cloud-based iBPMS IT SDK solution, together with standards and practices for use by healthcare providers subject matter experts (SMEs), as the Cloud Healthcare Appliance Real-Time Solution as a Service Reference Architecture or CHARTSaaS RA™; which is described according to the CHART acronym thus:
- Cloud-based – a solution-as-a-service (SaaS) integrated suite of software components, accessible anytime/anywhere via a secure portal;
- Healthcare – designed to support the extreme non-functional/system and functional/capability requirements of the healthcare provider domain;
- Appliance – a SDK intended for hands-on use by healthcare provider SMEs, both administrative and clinical, to create customized cognitive support apps with minimal cost and minimal need for IT staff support because of its data-driven/non-programming capabilities; and
- Real-Time – constantly and instantly available, to automate analytics-based cognitive support use cases that are time-sensitive and randomly occurring (e.g. – physiological device monitoring to minimize alarm/alert fatigue, immediate post-workup differential diagnosis to minimize diagnostic error and to maximize treatment plan effectiveness, etc.).
A more complete description of CHARTSaaS can be found here:
An IT configuration conforming to the CHARTSaaS RA would enable healthcare provider SMEs to design, develop, deploy, monitor and modify for continuous process improvement a wide variety of automated processes that might include any/all of these capabilities: complex event monitoring and analysis, Boolean and table-driven decision-making, Bayesian and multi-variate natural language dataset searching and record selection, and similarity and predictive analytics based on selected records or any accessible dataset/database. Also included is a capability for connectivity to and interoperability with any IT system-/staff-implicated actors that are accessible via cable or Wi-Fi communication facilities; such as staff communication via mobile device, access to and incorporation of data from a hospital information system (HIS) or electronic health record (EHR) system; installed on the user organization’s premises or geographically remote or in the Cloud.
A more complete example of the CHARTSaaS RA can be found here:
The following example serves to clarify the utility of a CHARTSaaS RA-compliant IT configuration for creation of customized and use case-specific applications, a.k.a. apps. A sentinel event, as reported to The Joint Commission (TJC) per TJC accreditation requirements and described in the April 2015 issue of TJC’s The Source, “… involved a patient whose blood levels were not drawn frequently enough to monitor the thinness of her blood while receiving a continuous heparin infusion. The patient had been started on a heparin infusion on an orthopedic unit and then was later transferred to a cardiac unit. The order set for the heparin infusion was not entered properly, leaving out the automatic order for blood tests every 6 hours. During the handoff report, the nurses did not discuss when the next blood test would occur to monitor the heparin infusion. For 24 hours, the patient went without blood tests until an oncoming nurse questioned the situation during the handoff report. At this time, the off-going nurse also reported that the patient had been complaining of a headache for several hours. A computerized tomography (CT) scan showed intracerebral hemorrhage. When the patient’s mental status deteriorated, the family chose not to proceed with surgery due to the patient’s multiple comorbidities and recent decrease in quality of life. She expired three days later.”[7]
Using an app built with a CHARTSaaS RA-compliant software suite, the previously installed EHR could have been monitored continuously (i.e. – 24 × 7 × 365) for occurrence and content of test order/result updates in the subject patient’s record. In the case of this sentinel event, the CHART-built app would have detected non-performance of the required test of patient blood coagulation capability, because the EHR would not have been updated with a ordered test result within the required elapsed timeframe from the time of the order; and the app would have notified clinical staff member(s) as specified in the app’s automated process description via his/her/their desktop, laptop and/or mobile digital device(s). Thus, the cognitive error of omission (in this case failures to communicate the order, to perform the required test and to react to the results in an appropriate and timely fashion) would have been avoided; and the patient’s life would have been saved. In addition, because the process was automated it could be modified using Lean/Six-Sigma tools and methods such as those described in TJC’s Robust Process Improvement (RPI)® [8] analysis methodology. Following application of RPI changes would be made by healthcare provider SMEs to the app software code (essentially executable documentation) for repeatable and reliable execution in subsequent similar situations, without the need for traditional document modification and the retraining of all staff who might be implicated in the future occurrences of the process.
In the urgent interest of transforming medical practice and healthcare delivery so as to mitigate medical mistakes and thereby to minimize the severity of consequent patient adverse events, we strongly recommend that healthcare providers investigate and develop or subscribe to CHARTSaaS RA-compliant IT configurations for the design, development and deployment of customized cognitive support apps. Patient lives hang in the balance.
[1] Bohmer RMJ. Perspective: The Hard Work of Health Care Transformation. N Engl J Med 2016;375:709-711.
[2] Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ 2016;353:i2139.
[3] Mandl KD, Kohane IS. Escaping the EHR Trap — The Future of Health IT. N Engl J Med 2012; 366:2240-2242.
[4] For example: Croskerry P. Diagnostic Failure: A Cognitive and Affective Approach appearing in Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology) Henriksen K, Battles JB, Marks ES, et al., editors, Rockville (MD) Agency for Healthcare Research and Quality (US); 2005 Feb.; and Groopman J. How Doctors Think. Houghton Mifflin Harcourt (New York, NY, 2008).
[5] Bohmer RMJ. Designing Care – Aligning the Nature and Management of Health Care. Harvard Business Press (Boston, MA, 2009), pp. 105-107, 128-133.
[6] Dunie R et al. Quadrant for Intelligent Business Process Management Suites. Gartner 18 August 2016 ID: G00276892 (http://www.gartner.com/doc/reprints?id=1-3F1C5YC&ct=160817&st=sb, viewed on 10/10/2016); and Rymer JR et al. The Forrester Wave™: Low-code Development Platforms, Q2 2016. Forrester 14 April 2016 (http://reprints.forrester.com/#/assets/2/85/%27RES117623%27/reports, viewed on 10/11/2016).
[7] The Joint Commission, The Source, Human Factors Analysis in Patient Safety Systems, XIII:4, April, 2015, p. 1, http://www.jointcommission.org/assets/1/6/HumanFactorsThe_Source.pdf
[8] Joint Commission Center for Transforming Healthcare, http://www.centerfortransforminghealthcare.org/about/rpi.aspx