
N.B. — This post is based on one of the continuously expanding roster of Actionable Patient Safety Solutions (APSS) a.k.a. “Challenges” as defined and described by the Patient Safety Movement Foundation (PSMF) and published at its web site (http://patientsafetymovement.org/challenges-solutions/actionable-patient-safety-solutions-apss/). Because the Foundation has set a goal of Zero Preventable Patient Deaths by 2020 (http://patientsafetymovement.org/), these APSS are understood to represent the most significant patient safety exposures created by medical mistakes, and medical mistakes are the third most frequent cause of patient deaths following heart disease and cancer (http://www.bmj.com/content/353/bmj.i2139).
“Accurate and complete hand-off communications (HOC) are vital to patient safety. When HOC information is incomplete or erroneous, serious patient harm often occurs. The establishment of accurate, complete, effective HOC requires an implementation plan that includes the following actionable steps:
- Hospital governance must become aware of this major performance gap as it exists in their own organization, and must participate in and support the following actions.
- Establish an HOC core team that includes a strong sponsor (senior clinical leadership is recommended for this role), physician champion, nursing champion and project leader. Other members will include practicing physicians, nurses, therapists, technicians and information technology experts.
- Define the exact roles of the sender and receiver in each category of HOC in order to make them effective and reliable.
- Educate all hospital staff on the following principles and requirements for effective HOC:
- HOC’s occur whenever patient care is transferred to a different caregiver, care team, hospital unit, or patient care site. Each HOC involves a ‘sender’ and a ‘receiver.’
- HOC failures occurs when (1) the ‘sender’ omits vital patient information from his/her report, or (2) the “receiver” fails to understand or properly record vital information given by the sender.
- A systematic, complete HOC process is similar in many ways to the pre-takeoff and pre-landing procedures used by aircraft crew. Aviation has made great progress in Quality Improvement in these procedures through the use of checklists. We will use a similar approach here.
- We have identified seventeen different categories of HOC that commonly occur in hospitals or other care units. Each of these categories requires a specific HOC checklist. We have developed the first 6, ready to be implemented:
- 1b – Emergency Department to Operating Room (Appendix A);
- 2f – Hospital Unit to Home (discharge) (Appendix B);
- 2g – Hospital Unit Shift Change (Appendix C);
- 3b – Operating Room to Hospital Unit (Appendix D);
- 3c – Operating Room to Home (Appendix E);
- 4c– Hospital to Outside Care Unit (Appendix F).
- Measure the effectiveness of current hand-off communication processes and build in to performance goals.”
The foregoing quote constitutes the “Executive Summary Checklist” from the above-captioned PSMF APSS Challenge #6 (http://patientsafetymovement.org/challenge/hand-off-communications/). Following is a case study of a fatal Patient Safety Sentinel Event, described in an article entitled “Human Factors Analysis in Patient Safety Systems,” appearing in a recent edition of a publication of The Joint Commission. The case is an example of a Handoff Communications (HOC) error, and it describeds a typical opportunity for patient safety optimization using information technology (IT) enabled cognitive support.
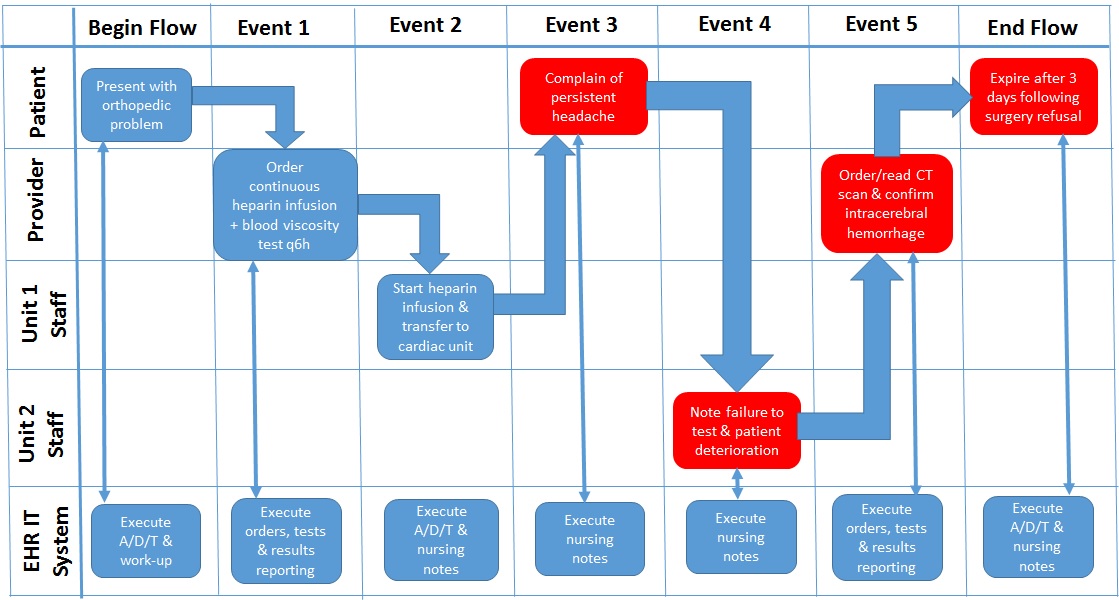
“A health care system submitted a root cause analysis (RCA) to The Joint Commission for a sentinel event that involved a patient whose blood levels were not drawn frequently enough to monitor the thinness of her blood while receiving a continuous heparin infusion. The patient had been started on a heparin infusion on an orthopedic unit and then was later transferred to a cardiac unit. The order set for the heparin infusion was not entered properly, leaving out the automatic order for blood tests every 6 hours. During the handoff report, the nurses did not discuss when the next blood test would occur to monitor the heparin infusion. For 24 hours, the patient went without blood tests until an oncoming nurse questioned the situation during the handoff report. At this time, the off-going nurse also reported that the patient had been complaining of a headache for several hours. A computerized tomography (CT) scan showed intracerebral hemorrhage. When the patient’s mental status deteriorated, the family chose not to proceed with surgery due to the patient’s multiple comorbidities and recent decrease in quality of life. She expired three days later. Although the organization had conducted a thorough RCA, The Joint Commission asked it to revise the RCA and consider human factors issues that led to the event and implement more strategies that incorporate human factors solutions, which would more reliably prevent the event from occurring again.”10
The patient monitoring fatal sentinel event activity flow described in foregoing case study is depicted the “As Is” process diagram in Figure 1.
Figure 1 – “As Is” Manual/EHR-Supported Patient Monitoring Process
If however, an IT solution had been available either on-site at the reporting healthcare system premises or by subscription to a CHARTSaaS in the cloud (an Internet-accessible and professionally managed data center), then such a tool could have been specified in The Joint Commission’s Patient Safety System Standard. Therefore, the Commission could have required an automation of the patient monitoring use case as a specific strategy in its request “… to revise the RCA [root cause analysis] and consider human factors issues that led to the event and implement more strategies that incorporate human factors solutions, which would more reliably prevent the event from occurring again.” Subsequently then, the CiBPMS-developed automated use case would be running continuously and/or conditionally per its healthcare provider SME-specified design. For the next instance of patient monitoring as described in the RCA report, CiBPMS-created automated use case could have recognized the failure to perform blood viscosity tests q6h, alerted staff of the omission, and prevented the patient’s death. This “To Be” process is depicted in Figure 2.
Figure 2 – “To-Be”CHARTSaaS-created Patient Monitoring Process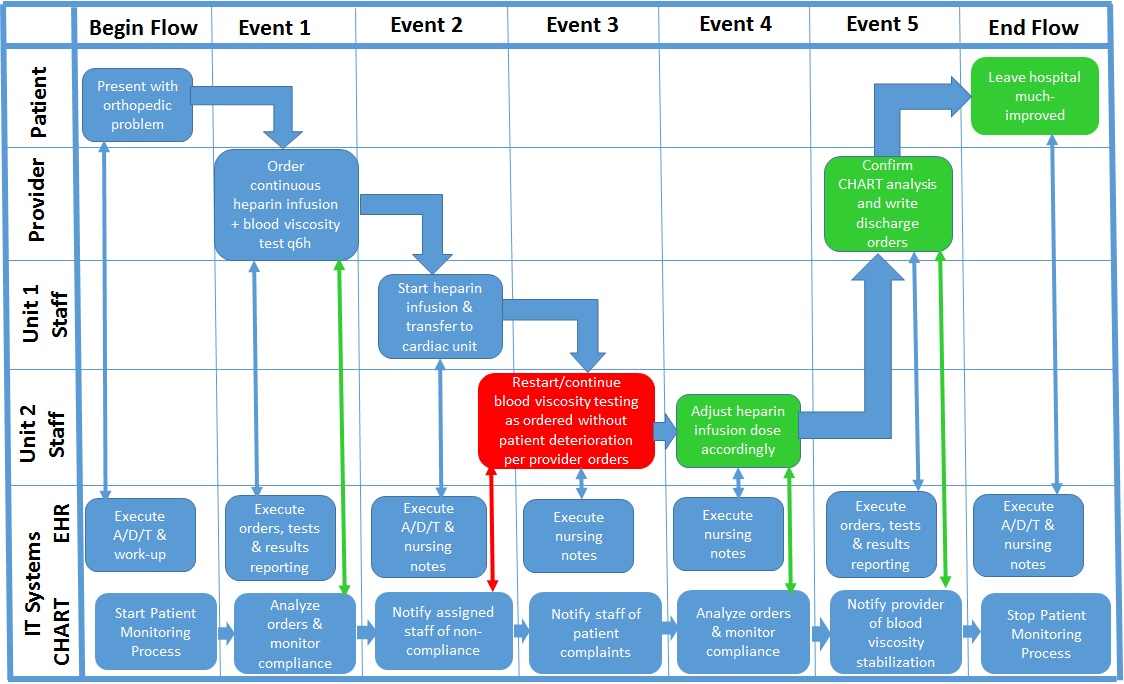
Reliable medical mistake mitigation and consequent patient adverse event avoidance require clinical cognitive support that only an IT solution such as CHARTSaaS can create, if employed by innovative healthcare provider subject matter experts. Please validate this proposition to your own satisfaction by reviewing the details of the Cloud Healthcare Appliance Real-Time Solution as a Service (CHARTSaaS) and its reference architecture in these presentations and imagining an IT solution even more effective than that proposed: