“Health care organizations have an absolute responsibility to deliver safe, reliable, and effective care to patients. Yet consistently meeting this obligation can be daunting, and organizations are often challenged to design a balanced portfolio of improvement projects that will enable them to meet system-level quality and safety goals. They may have stand-alone safety improvement projects underway, or regularly conduct staff surveys to better understand the organization’s current safety culture, but it remains unclear how these various efforts interweave and interact to provide safer, more reliable care. Diverse data streams are difficult to combine, making it challenging to develop sustainable, system-wide programs focused on all-cause harms and errors.
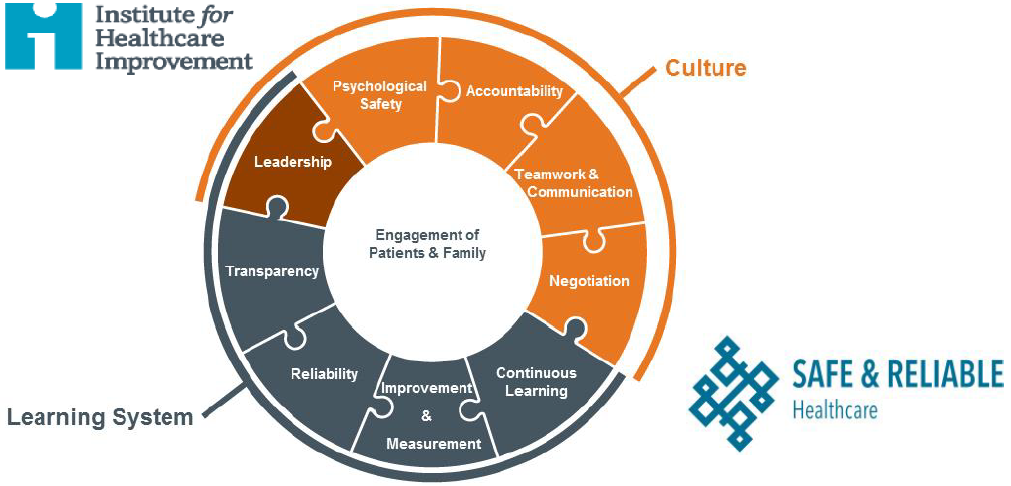
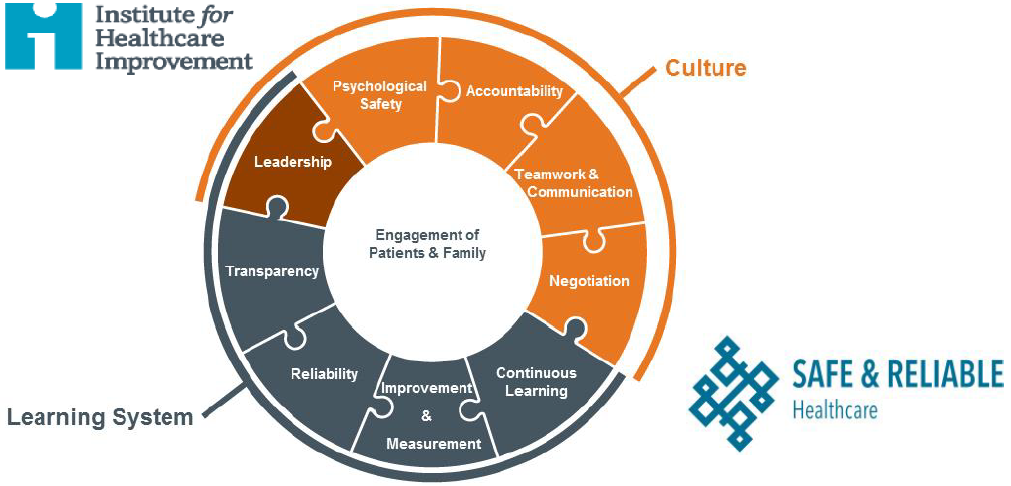
The Framework for Safe, Reliable, and Effective Care provides clarity and direction to health care organizations on the key strategic, clinical, and operational components involved in achieving safe and reliable operational excellence. It comprises two foundational domains — culture and the learning system — along with nine interrelated components: leadership, psychological safety, accountability, teamwork and communication, negotiation, transparency, reliability, improvement and measurement, and continuous learning. Engagement of patients and their families is at the core of the framework — the engine that drives the focus of the work to create safe, reliable, and effective care.”
The foregoing quote is from the white paper entitled A Framework for Safe, Reliable, and Effective Care authored by a group of subject-matter experts at the Institute for Healthcare Improvement (IHI) and Safe & Reliable Healthcare (SRH) resulting from a fifteen-year collaboration (Frankel A, Haraden C, Federico F, Lenoci-Edwards J. A Framework for Safe, Reliable, and Effective Care. White Paper. Cambridge, MA: Institute for Healthcare Improvement and Safe & Reliable Healthcare; 2017; http://www.ihi.org/resources/_layouts/download.aspx?SourceURL=/resources/Knowledge+Center+Assets/IHIWhitePapers+-+AFrameworkforSafeReliableandEffectiveCare_d9247dfc-09ac-4777-bef1-62c7c9bd604c/FrameworkSafeReliableEffectiveCareWhitePaper.pdf). Although the paper proposes an apparently complete taxonomy — nine components including “leadership, psychological safety, accountability, teamwork and communication, negotiation, transparency, reliability, improvement and measurement, and continuous learning” and comprising two “foundational domains” called “culture” and “the learning system” — provides a useful intellectual framework to consider safe, reliable and effective care, it appears not to contribute anything novel regarding the mitigation of medical mistakes and consequent patient safety improvement beyond the findings and deliverables being produced continually by such institutions as the Armstrong Institute for Patient Safety and Quality at Johns Hopkins (http://www.hopkinsmedicine.org/armstrong_institute/) or the Ariadne Labs at Brigham and Women’s Hospital and the Harvard T. H Chan School of Public Health (https://www.ariadnelabs.org/). However, this included description of the “reliability” component is an excellent statement of purpose and requirements for a much-needed patient safety system:
“Reliability is the ability of a system to successfully produce a product to specification repeatedly. In the case of health care, that product is safe, efficient, person-centered care. The challenge in achieving reliability in health care is the complexity of the processes, which heavily depend on human beings and their interactions with each other. Vigilance and exhortation are inadequate to counter human foibles, and sometimes good people err and the consequences can be dire. Great organizations design systems that take advantage of people’s intrinsic strengths and support their inherent weaknesses, and in doing so increase the likelihood of reliable performance. Mediocre organizations, by comparison, assume that vigilance and intrinsic strengths overcome human fallibility and inherent personal and organizational weaknesses.
To achieve high levels of reliability across processes and systems, organizations must apply best evidence and minimize non-patient-specific variation, with the goal of failure-free operation over time. This is the science of reliability.
There are four foundational principles for making systems and processes more reliable:
- Standardize: This involves designing processes so that people do the same thing the same way every time. Standardization makes it easier to train people on the processes, and it becomes more apparent if the processes fail and where they fail, enabling the organization to better target improvements.
- Simplify: The more complex something is, the less likely it is to be successful because there are more opportunities for mistakes, and staff may avoid following processes that are too difficult or time consuming. Simplified processes, however, make it easy for people to do the right thing.
- Reduce autonomy: Health care professionals have historically been autonomous, making decisions based on personal preference or an individualized belief in their perspective. However, this can result in care variation and less consistent outcomes. To achieve greater reliability, organizations must set the expectation that care delivery follows evidence-based best practices, unless contraindicated for specific patients.
- Highlight deviation from practice: Clinicians sometimes have good reasons for departing from standardized processes. Smart health care organizations create environments in which clinicians can apply their expertise intelligently and deviate from protocols when necessary, but also relentlessly capture the deviations for analysis. Once analyzed, the new insights can lead to educating clinicians or altering the protocol. Both result in greater reliability.
When contraindications exist, health care professionals need to document the reasons why departing from standard care practice is warranted, so that the organization can learn and determine whether the process should be modified. For example, for patients on a ventilator, there is evidence that the head of the bed should be elevated between 30 and 45 degrees. For most patients, this is the right thing to do. However, there are some individuals who, because of their medical situation or characteristics specific to them, will not benefit from an elevated head of the bed. In these cases it is okay to depart from best practice, provided the patient’s treatment team has duly considered the evidence-based care and documented the reasons why they’re choosing to follow another method.
For most clinical conditions and situations, there is evidence-based care that patients should receive every time, unless contraindicated. When evidence does not dictate a particular care path, clinicians need to work together to identify the simplest and most reliable path and agree to abide by the group’s decisions. In so doing, they simplify the care pathway, enabling organizations to be more efficient and making care more reliable. As new evidence develops, care pathways must be reviewed periodically to ensure that the agreed-upon care practices remain relevant.”
An information technology (IT) solution compatible with the Cloud Healthcare Appliance Real-Time Solution as a Service Reference Architecture (CHARTSaaS RA) can be used by healthcare provider subject matter experts to create IT applications, a.k.a.”apps,” that meet the requirements of the Reliability component specified in the foregoing excerpt from the IHI-SRH whitepaper. Please validate this automated process proposition to your own satisfaction by reviewing the details of CHARTSaaS and the CHARTSaaS RA in these presentations, and then by imagining a CHARTSaaS-enabled IT solution:
Healthcare providers and their patients will benefit significantly from appreciating and then applying a CHARTSaaS RA-compliant IT solution. To do so will mitigate medical mistakes (currently the third leading cause of patient deaths, per Makaray and Daniel, http://www.bmj.com/content/353/bmj.i2139), thereby minimizing patient adverse events; and also will optimize clinical case outcomes while maximizing the cost-effectiveness of care and treatment and accelerating the accrual of medical knowledge.